The most common form of arthritis, affecting millions of people worldwide.Rheumatoid arthritis - the second most common form of arthritis - affects other parts of the body besides the joints.A joint disease that mostly affects cartilage,the slippery tissue that covers the ends of bones in a joint that breaks down and wears away over time.In a normal joints,a healthy cartilage is a firm,slippery tissue provides a smooth, gliding surface for joint motion and acts as a cushion. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. As OA worsens over time, bones may break down and develop growths called spurs. Bits of bone or cartilage can break off and float inside the joint space, which causes more pain and damage.It can damage any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe.Occurs in people of all ages, osteoarthritis is most common in people older than 65(usually begins later in life). Common risk factors include increasing age, obesity, previous joint injury, overuse of the joint, weak thigh muscles, and genes.Osteoarthritis often gradually worsens, and no known cure .Progression can be slow dow by maintaining a healthy weight and other treatments. Osteoarthritis symptoms often develop slowly and worsen over time. >1.Pain - tends to be worse when you move your joint or at the end of the day.May feel pain more often in severe cases.Example is hip pain felt in the groin area or buttocks and sometimes on the inside of the knee or thigh. 2.Tenderness - may feel tender when you apply light pressure to it.Pain and tenderness is felt in the large joint at the base of the big toe. There may be swelling in ankles or toes.
3.Stiffness - most noticeable particularly first thing in the morning or after a period of inactivity.Joints may feel stiff after rest, but this usually wears off as you get moving.
4.Swelling – affected joints may get swollen, especially after extended activity.The swelling may be hard (caused by osteophytes) or soft (caused by synovial thickening and extra fluid), and the muscles around your joint may look thin or wasted.
5.Grating sensation - may hear or feel a grating sensation when you use the joint.A grinding sensation (crepitus).A “grating” or “scraping” sensation occurs when moving the knee.
6.Loss of flexibility - may not be able to move your joint through its full range of motion.
7.Bone spurs - extra bits of bone, which feel like hard lumps, may form around the affected joint.Bony growths (spurs) at the edge of joints can cause fingers to become swollen, tender and red. There may be pain at the base of the thumb.

Image Source
https://goo.gl/images/1Ht7Tc
Risk Factors: Who may get this?
1.Older age - occurs most often in older people but younger people sometimes get osteoarthritis primarily from joint injuries.usually starts from the late 40s onwards.Not fully understand why it’s more common in older people, but it might be due to your muscles weakening and your body being less able to heal itself, or your joint slowly wearing out over time. -
2.Gender - women are more likely to develop osteoarthritis, though it isn't clear why.For most joints, especially the knees and hands, osteoarthritis is more common and more severe in women.
3.Obesity - many years of carrying extra pounds can cause the cartilage that cushions joints to break down faster.It puts added stress on weight-bearing joints, such as your hips and knees.
4.Genetics - various genetic traits can make a person more likely to develop OA. One possibility is a rare defect in the body’s production of collagen, the protein that makes up cartilage.
5.Joint injuries and overuse(trauma) - repetitive movements or injuries to joints (such as a fracture, surgery or ligament tears) can lead to osteoarthritis. Some athletes, for example, repeatedly damage joints, tendons and ligaments, which can speed cartilage breakdown. Injuries, such as those that occur when playing sports or from an accident, may increase the risk of osteoarthritis.
6.Certain occupations - stresses on the joints from certain jobs and playing sports.Certain careers that require standing for long periods of time, repetitive bending, heavy lifting or other movements can also make cartilage wear away more quickly. An imbalance or weakness of the muscles supporting a joint can also lead to altered movement and eventual cartilage breakdown in joints.
7.Bone deformities/Joint abnormalities - were born with abnormalities or with malformed joints or defective cartilage, which can increase the risk of osteoarthritis.Perthes’ disease of the hips is an example.
8.Other diseases - having diabetes or other rheumatic diseases such as gout and rheumatoid arthritis can increase your risk of osteoarthritis.Certain metabolic disorders such as hemochromatosis, which causes the body to absorb too much iron, or acromegaly, which causes the body to make too much growth hormone.
Complications
1.Gout - a common type of inflammatory arthritis, which is caused by high levels of urate that lead to sodium urate crystals forming in and around your joints. The changes that osteoarthritis causes in cartilage can encourage crystals to form within your joint. If you have both osteoarthritis and a high level of urate in your blood, you’re at an increased risk of developing gout.
The base of the big toe is a very common site for a painful attack of gout, and this is partly because this joint is the most common joint in the foot to be affected by osteoarthritis.
2.Chondrocalcinosis - a calcium pyrophosphate crystals formed in your cartilage.OA tends to become more severe more quickly when calcium crystals are present.
3.Diabetes and Heart Disease - knee or hip pain may lead to a sedentary lifestyle that promotes weight gain and possible obesity. Being overweight or obese can lead to the development of diabetes, heart disease and high blood pressure.
4.Falls - people with osteoarthritis experience as much as 30 percent more falls and have a 20 percent greater risk of facture than those without OA. People with OA have risk factors such as decreased function, muscle weakness and impaired balance that make them more likely to fall. Side effects from medications used for pain relief can also contribute to falls. Narcotic pain relievers can cause people to feel dizzy and unbalanced.
Diagnosis
No single test can diagnose osteoarthritis. Most doctors use several methods, including medical history, a physical exam, x-rays, or lab tests.A doctor will collect information on personal and family medical history, perform a physical examination and order diagnostic tests.
1. Patient Health History and Symptoms
a. Detailed description of the symptoms.
b. When did your joint pain or other symptoms begin?Is the pain continuous, or does it come and go
c. Information about medical problems you've had.Have you ever injured this joint?
d. Location of the pain, stiffness or other symptoms.Visual inspection.
e. How the symptoms affect daily activities or any particular activities make the pain better or worse?
f. Information about the medical problems of your parents or siblings.
g. All the prescription and over-the-counter medications and dietary supplements you take and the dosages
h. List of current medications.
2. Physical Examination
a. Examination of the joints - look for joint damage,tenderness, pain, or swelling; body mechanics.
b. X-ray - cam show damage and other changes related to osteoarthritis. Cartilage loss is revealed by a narrowing of the space between the bones in your joint.
c. Blood test - are usually not helpful in a diagnosis. May help rule out other causes of joint pain, such as rheumatoid arthritis.
d. Joint aspiration - involves withdrawing (aspirating) a sample of fluid from a joint using a needle and syringe either relieve swelling or to obtain fluid for analysis to diagnose a joint disorder and/or problem.
e.Magnetic resonance imaging (MRI) - isn't commonly needed to diagnose osteoarthritis but may help provide more information in complex cases. Produce detailed images of bone and soft tissues, including cartilage.

Presentation of a healthy and a diseased joint
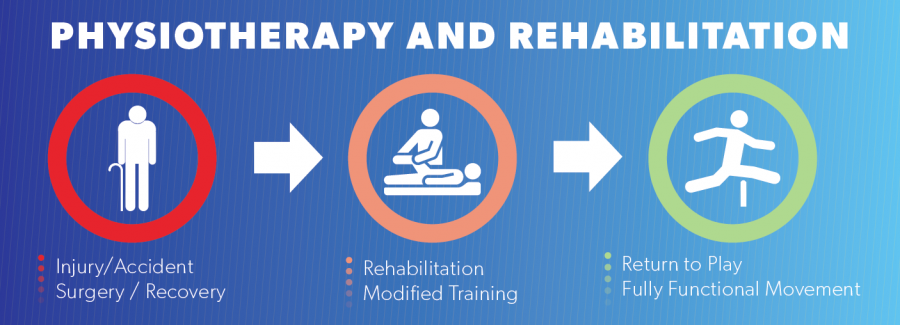
Treatment Goals and Intervention
1. Managing symptoms, such as pain, stiffness and swelling -Transcutaneous electrical nerve stimulation (TENS) can help to ease pain. Heat and cold therapies.
2. Improving joint mobility and flexibility - Range-of-motion exercise helps maintain and improve joint flexibility and reduce stiffness. Slow, gentle stretching of joints may improve flexibility, lessen stiffness and reduce pain. Yoga and tai chi are great ways to manage stiffness.
3. Maintaining a healthy weight - excess weight adds additional stress to weight-bearing joints, such as the hips, knees, feet and back. Appropriate diet with increased physical activity will effectively loss weight. One of the most beneficial ways to manage OA is to get moving.
4. Getting enough of exercise -The U.S. Department of Health and Human Services recommends that everyone, including those with arthritis, get 150 minutes of moderate exercise per week. Strengthening exercises to muscles around the affected joints.
5. Physical Activity - Aerobic exercise helps to improve stamina and energy levels and also help to reduce excess weight. Walking, gardening, briskly pushing a baby stroller, climbing the stairs, playing soccer, or dancing the night away are all good examples of being active.
6. Assistive devices -Braces or shoe inserts can help reduce pain when you stand or walk. It can immobilize or support your joint to help take pressure off it as well as help with function and mobility. These include items, such as like scooters, canes, walkers, splints, shoe orthotics or helpful tools, such as jar openers, long-handled shoe horns or steering wheel grips.

Pain and Anti-inflammatory Medications
Medicines for osteoarthritis are available as pills, syrups, creams or lotions, or they are injected into a joint. They include:
1. Analgesics. These are pain relievers and include acetaminophen, opioids (narcotics) and an atypical opioid called tramadol. They are available over-the-counter or by prescription. Acetaminophen (Tylenol, others) can relieve pain, but it doesn't reduce inflammation. It has been shown to be effective for people with osteoarthritis who have mild to moderate pain. Liver damage if taken more than the recommended dosage.
2. Nonsteroidal anti-inflammatory drugs (NSAIDs). These are the most commonly used drugs to reduce inflammation and relieve pain. They are available over-the-counter(ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve, others) or by prescription(stronger NSAID). Side effects include stomach upset, ringing in your ears, cardiovascular problems, bleeding problems, and liver and kidney damage. Oral NSAIDs has more side effects compared to topical NSAIDs. Oral NSAIDs usually not recommended to older people over 65 years of age and those with stomach bleeding.
3. Corticosteroids. These are powerful anti-inflammatory medicines taken by mouth or injected directly into a joint. It can start to work within a day or so and may improve pain for several weeks or even months. Steroid injections are mainly used: • for very painful osteoarthritis; for sudden, painful attacks; to help you through an important event (such as a holiday or family wedding)
Complementary and Alternative Medicine
These include nutritional supplements, acupuncture or acupressure, massage, relaxation techniques and hydrotherapy, among others.
Surgery
Joint surgery can repair or replace severely damaged joints, especially hips or knees performed by an orthopaedic surgeon.Surgery can be recommended if pain is very severe or you have mobility problems or if conservative treatments don't help. Some surgical procedure may include osteotomy and arthroplasty.
Helpful site:
Common aches and pain
See more at: http://www.arthritisresearchuk.org/arthritis-information/common-pain.aspx
Exercises to manage pain
See more at: http://www.arthritisresearchuk.org/arthritis-information/exercises-to-manage-pain.aspx